WASHINGTON, DC – An independent advisory committee for the Food and Drug Administration (FDA) will meet on July 13 to review a new Alzheimer’s drug, a decision that holds profound implications for millions of patients and their families.
- Crucial FDA Meeting – An FDA advisory committee will convene on July 13, 2025, to assess the safety and efficacy of “Neurovance,” a new investigational drug for early-stage Alzheimer’s disease.
- The Human Toll – More than 6 million Americans are currently living with Alzheimer’s, a number projected by the Alzheimer’s Association to rise to nearly 13 million by 2050.
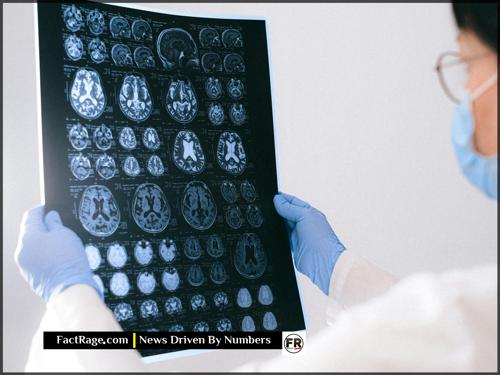
- The Science of Hope – Developed by Synaptic Therapeutics, Neurovance is an antibody treatment that targets amyloid plaques, reportedly slowing cognitive decline by 35% in Phase 3 trials with a potentially improved safety profile over existing medications.
Behind the clinical data and regulatory procedures lies a landscape of human experience, where families navigate the daily realities of a disease that erodes memory and identity, pinning their hopes on the outcome of meetings like this one.
The Anatomy of Hope
![]() It’s easy to view a story like this through the lens of data points and regulatory acronyms. Yet, beneath the statistics and procedures lies a more universal narrative about what it means to wait—to pin the possibility of more time with a loved one on the slow, uncertain, and deliberate march of science. This story explores that intersection, reminding us that at the center of every potential medical breakthrough is the profoundly human landscape of hope.
It’s easy to view a story like this through the lens of data points and regulatory acronyms. Yet, beneath the statistics and procedures lies a more universal narrative about what it means to wait—to pin the possibility of more time with a loved one on the slow, uncertain, and deliberate march of science. This story explores that intersection, reminding us that at the center of every potential medical breakthrough is the profoundly human landscape of hope.
The Weight of Waiting for a Breakthrough
For Sarah Jenkins, a 45-year-old graphic designer from Ohio, the July 13th meeting is more than an event on a news calendar. It’s a focal point of hope. Her father, Michael, a 68-year-old retired history teacher, was diagnosed with early-onset Alzheimer’s three years ago. His diagnosis transformed their family, turning Sarah into a part-time caregiver who watches the man who taught her about the world slowly lose his connection to it.
“Some days are good. We’ll talk about old movies, and he’s right there with me,” Sarah explains. “Then there are days he doesn’t recognize the house he’s lived in for 40 years. You’re constantly grieving someone who is still here.” The family follows news of every potential treatment with a mix of cautious optimism and exhaustion. A drug that could slow the disease’s progression, even modestly, represents the chance for more good days—more time with the father she knows.
What Makes ‘Neurovance’ a Potential Game-Changer?
The drug at the center of this hope is Neurovance, developed by the privately held biotech firm Synaptic Therapeutics. Like some recently approved treatments, it is a monoclonal antibody designed to clear amyloid-beta plaques, the toxic protein clumps in the brain that are a hallmark of Alzheimer’s disease. So, what makes this one different?
According to data released by the company, participants in its Phase 3 clinical trial who received Neurovance showed a 35% slower rate of cognitive decline compared to those on a placebo. Proponents also point to its safety profile. A key concern with similar amyloid-targeting drugs is a side effect known as ARIA (amyloid-related imaging abnormalities), which can cause brain swelling or bleeding. Synaptic Therapeutics reported a lower incidence of ARIA in its trials compared to other drugs in its class, a detail the FDA committee is certain to scrutinize heavily.
The High-Stakes Path to Approval
The advisory committee’s task is to weigh these potential benefits against the risks. The panel of independent experts will pour over thousands of pages of trial data, debating the clinical significance of the 35% slowdown and questioning the company’s representatives on the drug’s safety. Their final vote is a recommendation, not a binding order, but the FDA gives it significant weight and usually follows its advice.
The memory of past controversies, such as the contentious approval of another Alzheimer’s drug, Aduhelm, looms over the proceedings, ensuring this review will be exceptionally thorough. For the scientific community, it is a test of a leading theory of Alzheimer’s treatment. For Synaptic Therapeutics, it is a critical business milestone. But for Sarah Jenkins and millions like her, the outcome is far more fundamental. It is about the possibility of more time.
More Than a Molecule
![]() On July 13th, a committee will weigh clinical data, but for families like the Jenkinses, the true measure is in moments—past, present, and the potential for a different future. The verdict on Neurovance will be a regulatory one, but its resonance is profoundly human, a testament to the universal search for hope within the intricate landscape of medicine. It is a story that reveals how deeply our lives are intertwined with the slow, steady, and uncertain march of science.
On July 13th, a committee will weigh clinical data, but for families like the Jenkinses, the true measure is in moments—past, present, and the potential for a different future. The verdict on Neurovance will be a regulatory one, but its resonance is profoundly human, a testament to the universal search for hope within the intricate landscape of medicine. It is a story that reveals how deeply our lives are intertwined with the slow, steady, and uncertain march of science.